Trigger Point Injection
Trigger point injection is a procedure used to treat painful areas of muscle that contain trigger points, or knots of muscle that form when muscles do not relax. Many times, such knots can be felt under the skin. Trigger points may irritate the nerves around them and cause referred pain, or pain that is felt in another part of the body.
Introduction
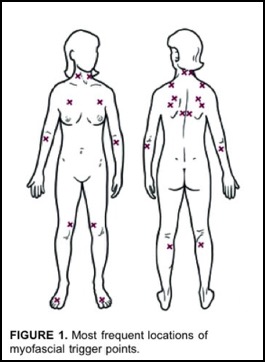
Trigger points (see Figure 1) are classified as being active or latent, depending on their clinical characteristics. An active trigger point causes pain at rest. It is tender to palpation with a referred pain pattern that is similar to the patient’s pain complaint. This referred pain is felt not at the site of the trigger point origin, but remote from it. The pain is often described as spreading or radiating. Referred pain is an important characteristic of a trigger point. A latent trigger point does not cause spontaneous pain, but may restrict movement or cause muscle weakness. The patient presenting with muscle restriction or weakness may become aware of pain originating from a latent trigger point only when pressure is applied directly over the point.
Pathogenesis
Many researchers agree that acute trauma or repetitive microtrauma may lead to the development of a trigger point. Lack of exercise, prolonged poor posture, vitamin deficiencies, sleep disturbances, and joint problems may all predispose to the development of microtrauma. Occupational or recreational activities that produce repetitive stress on a specific muscle or muscle group commonly cause chronic stress in muscle fibers, leading to trigger points. Examples of predisposing activities include holding a telephone receiver between the ear and shoulder to free arms; prolonged bending over a table; sitting in chairs with poor back support, improper height of arm rests or none at all; and moving boxes using improper body mechanics. Acute sports injuries caused by acute sprain or repetitive stress (e.g., pitcher’s or tennis elbow, golf shoulder), surgical scars, and tissues under tension frequently found after spinal surgery and hip replacement may also predispose a patient to the development of trigger points.
Clinical Presentation
Patients often report regional persistent pain resulting in decreased range of movement of the muscle in question, which are often muscles involved in maintaining posture. In the head and neck region, trigger point pain may manifest as tension headache, tinnitus, temporomandibular joint pain, eye symptoms or torticollis. In the arm, the pain may mimic bursitis or tendonitis, and in the legs the pain can be a cause of limited range of movement of the knee or ankle.
Evaluation
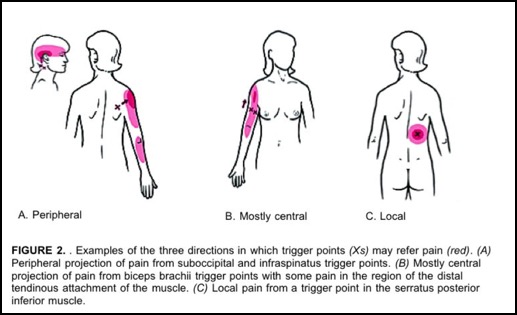
Palpation of a hypersensitive bundle or nodule of muscle fiber of harder than normal consistency is the physical finding most often associated with a trigger point. Localization of a trigger point is based on the physician's sense of feel, assisted by patient expressions of pain and by visual and palpable observations of local twitch response. This palpation will elicit pain over the palpated muscle and/or cause radiation of pain toward the zone of reference in addition to a twitch response. The commonly encountered locations of trigger points and their pain reference zones are consistent (see Figure 2).
Management
Trigger point injection can effectively inactivate trigger points and provide prompt, symptomatic relief. Injections are given in the physician’s office and takes approximately 30 minutes. A small needle is inserted into the trigger point and a local anesthetic (e.g., lidocaine, procaine) with or without vitamin B12 is injected. Injection of medication inactivates the trigger point and thus alleviates pain. Sustained relief usually is achieved with a brief course of treatment. The injection may cause a twitch or pain that last a few seconds to a few minutes.